The Latest Understanding, Treatment And Nutritional Intervention For Horses Experiencing Seasonal Skin & Respiratory Allergies
Much like the impact that seasonal allergies have on humans and their daily quality of life, horses are affected by both skin and respiratory allergies that go beyond simple discomfort to limit performance capacity, cause infection, alter behavior and, in severe cases, cause permanent damage to the skin and lungs.
Seasonal allergies are a constant frustration shared by horse owners and veterinarians. Their specific cause is often shrouded in mystery, and the breadth and effectiveness of available treatments are limited. There are, however, several insights gleaned from existing data, evolving research and anecdotal success seen by veterinarians that are offering relief to affected horses.
“My reason for going to nutrition is to get these horses off the corticosteroids as quickly as I can while using as little of them as I can.”
— Roland Thaler, VMD, Metamora Equine
What is an Allergy?
“Seasonal allergies are immune disorders characterized by hypersensitivity to specific substances,” explains Tara Hembrooke, PhD, MS, Research Scientist with Platinum Performance, Inc. “Most commonly,” she continues, “seasonal allergic reactions affect the skin and respiratory airways in horses and generally develop in response to exposure to insect bites, molds, spores and certain proteins present in pasture grasses.” Allergies are ubiquitous, meaning that potential causes are everywhere in the typical horse’s environment, making allergens difficult to avoid and pinpoint diagnostically. “The number one thing I try to do is first identify the problem and be as specific as I can,” says Roland Thaler, VMD, owner of Metamora Equine in Metamora, Michigan. “When I get a horse with a cough, runny eyes or increased respiratory effort, then I try to say ‘is this an allergy, a bacterial issue or a virus?’ ” Much like the struggle human physicians experience when trying to narrow down a specific allergen, equine veterinarians are faced with a seemingly endless list of suspects. What trees, grasses and pollens is the horse exposed to daily? Is the material in their stall contributing? Is the insect population under control? Is dust being kept at bay as much as possible? A veterinarian’s primary approach is very often an elimination strategy; slowly eliminating elements from a horse’s environment until symptoms improve and the cause of the allergic response can be determined, or at least narrowed. “This is very important,” says Cyprianna Swiderski, DVM, PhD, DACVIM, Associate Professor, Equine Medicine Department of Clinical Sciences at Mississippi State University. “In our treatment protocol, we first identify what the etiology is then, hopefully, eliminate it. That’s the ultimate goal.”
Managing the Seasonal Allergic Response
1. Veterinary Care
Veterinarians are best equipped to offer sound advice on maintaining a healthy environment, diet and supplement regimen for horses
2. Deal with Dust
Reduce dust by using stall materials that don’t generate excess dust, while keeping turnouts, paddocks and pastures adequately watered.
3. Aid with Insects
Fans and fly sprays are great tools to keep the insect population down and the prevalence of bites low. Fly sheets and masks can also help.
4. Proper Diet
Choose a diet based on high-quality forage with minimal grains and concentrates. Soak hay or use a hay steamer if necessary to minimize inhaled allergens.
5. Supplements
Choose one of Platinum’s foundational wellness formulas to help maintain overall health, normal allergic response and immune health in particular. For horses with advanced needs, add Platinum Skin & Allergy and, in some cases, Platinum's Healthy Weight oil.

The Immune System Component
With an allergic response being attributed to an immune system hypersensitivity, maintaining a healthy immune system becomes greatly important. “In addition to a balanced diet, supplementation with specific nutrients can help support the immune system,” says Dr. Hembrooke. The health of the equine immune system plays a role in virtually every other aspect of a horse’s overall health and, arguably, their performance as well. One of the most effective ways to maintain an optimally-functioning immune system is to provide the foundational support needed for optimal wellness; it’s one of the primary reasons Platinum Performance® was developed in clinical practice over 20 years ago. Paying close attention to a horse’s diet, then supplementing them with the missing pieces and more therapeutic nutrients lays the groundwork for horses to thrive long-term as healthier animals and more durable athletes.
“For me, I would rather take a nutritional approach. I think for the long-term you’re actually fixing a problem rather than putting a band-aid on it. If I can get the job done in a more functional way, and actually solve the problem, then we’re miles ahead.”
— Kim Gill-Favier, DVM
Skin Allergies & Insect Bite Hypersensitivity
Skin allergies are by far the most common type of seasonal allergies in horses, developing as a result of exposure to virtually anything the horse may come into contact with, from pollen, dust and mold to shampoos, fly spray and saddle pads. Although rare, skin allergies can also present as a reaction to certain grasses, grains, feed additives and supplements, and take on several forms. “Skin allergies may present as itchiness and possibly damage to skin like bald spots or scabs,” says Dr. Hembrooke. The intersection of the immune and nervous systems results in an itching sensation for affected horses, oftentimes resulting in loss of use until the allergic response can be mitigated. “Raised bumps that may or may not be itchy may be another sign,” continues Dr. Hembrooke, “and while skin allergies are mostly seen as a nuisance, they can result in infection if not controlled properly.” Kim Gill-Favier, DVM, shares the frustration of seasonal skin allergies, “The most common thing I see is urticaria, or hives. It always seems to come up in February and March when we’ve had a lot of rain, things are starting to bloom and there may be molds. Horses will start to have urticaria, which you treat once and it always seems to come back.”
Horse owners don’t necessarily equate a horse’s insect bites and the subsequent reaction to an allergic response, but in reality, horses can be predisposed to react more severely depending on the state of their immune system. Insect bite hypersensitivity (IBH) is the most prolific equine seasonal allergy, and subsequently, among the most extensively studied. Characterized by a skin reaction to bites from insects such as Culicoides, flies, mosquitos and other insects, IBH affects an incredibly large number of horses regardless of breed, age or discipline. “IBH is really a big problem,” says Dr. Thaler. “I don’t think we approach it strongly enough and fly spray just isn’t cutting it. We should be treating these horses proactively.” Aside from removing horses from an outside environment during times of prime insect activity, such as dawn and dusk, fans can be added to barns and stalls to help curb insect activity. Working from within the horse, their diet should be focused on maintaining normal levels of inflammation and maintaining a balanced immune system. High-quality forage with limited grains and concentrates plus a focus on omega-3 oils and supplemented omega-3 fatty acids and antioxidants can lay the groundwork for a horse that’s more equipped to handle the insult of insect bites.

Respiratory Allergies
The study of respiratory allergies in horses is advancing well beyond the limited understanding of decades past. A greater link between the horse’s environment and varying levels of respiratory distress has been made, leading to a change in nomenclature and stronger ties between the study of respiratory allergies in horses and humans. “We study what is now called equine asthma,” explains Dr. Swiderski. “And the first thing is to recognize that equine asthma is a syndrome that typically houses what was formerly known as inflammatory airway disease and also RAO, or recurrent airway obstruction.” There are two levels of severity when it comes to equine asthma, with the first being formerly known as equine inflammatory airway disease, and now referred to as mild to moderate asthma. The second was formerly regarded as RAO, and now deemed severe asthma. “With severe asthma, there are horses who go in the barn, they’re exposed to moldy hay, and that’s how they trigger that disease,” says Dr. Swiderski. “Researchers can actually trigger equine asthma by bedding horses on moldy hay.” Growing up in Maryland, Dr. Swiderski was shocked by the prevalence of severe asthma in the horses she saw when she moved to the southeastern United States. “These horses differed from the barn-associated disease I had grown up with, in that they experienced signs on pasture during conditions of high heat and humidity. I had never seen horses in so much distress,” she says, with a hint of sadness underlying the determination in her voice. “I’ve become passionate about equine asthma because my heart goes out to these horses that have no real way to escape from the pasture associated antigens that are triggering this disease that is chronic and progressive. Horses ultimately can die from it.”
Symptoms of the barn associated form of severe equine asthma can include nasal or ocular discharge, coughing or labored breathing, and can often be greatly impacted by modest changes to a horse’s environment. “I’ll first try to get this horse away from the dust,” says Dr. Thaler. “I’ll try to get [the barn associated horses] outside the barn, have their hay soaked to minimize what they’re inhaling from it, and I’ll have my clients add the right oil to the feed.” Choosing an oil, such as omega-3-rich flax oil, can support normal levels of inflammation. Beyond oils, short-term treatment with corticosteroids is commonplace to help get symptoms under control, as is the use of certain targeted nutrients for longer-term benefit. “My reason for going to nutrition is to get these horses off the corticosteroids as quickly as I can while using as little of them as I can,” says Dr. Thaler. “A lot of my show horses are pretty overweight, so for several reasons I try to use nutrition, and specifically, the Platinum Skin & Allergy formula.”
The Real Impact of Your Horse’s Diet
Inflammation is known to play a significant role in allergic response, however diet is perhaps one of the best ways to influence health and help support normal healthy inflammation in a horse’s body. “A primary goal is to establish or re-establish a proper balance between omega-6 fatty acids and omega-3 fatty acids,” says Dr. Hembrooke. “Oils high in omega-6 fatty acids, like corn and cottonseed, should be eliminated and replaced with oils high in omega-3 fatty acids. Antioxidants like vitamins E and C may help decrease oxidative damage in tissues. If there is a strong immune response, then there is going to be an increased production of free radical species that can be mediated with antioxidants. Quercetin is a powerful polyphenolic antioxidant that offers further natural support for allergies. Pro- and prebiotics should also be considered as they will support a healthy gut microbial population that is going to then support a healthy immune state.”
Starting with the right hay is crucial, but realizing exactly what nutrients hay is providing — and what it’s not — is equally as important. For instance, the level of omega-3 fatty acids and antioxidants in fresh, still growing alfalfa can be 38-40 percent higher than the same alfalfa just 6 weeks post-harvest. With nutrient rates diminishing over time in even the highest-quality hay, baled hay stops short of delivering all of the necessary nutrients horses need to function at their best, making supplementation an excellent choice. Foundational wellness and performance formulas like Platinum Performance® Equine, Platinum Performance® GI, Platinum Performance® DJ and Platinum Performance® CJ are recommended to support immune function and total body health because of their comprehensive levels of omega-3 fatty acids, vitamins and trace minerals. “We compared the allergic response to various known seasonal allergens, via intradermal injection, before and after 11 weeks of supplementation of omega-3 fatty acids, vitamins and trace minerals plus a hay diet,” says Dr. Hembrooke, explaining a research study using supplementation together with a high-quality, forage-based diet. “Each response was recorded at 30 minutes, 2 hours, 4 hours, 8 hours, 24 hours and 48 hours post-injection. We measured the size and feel of each wheal and compared it to positive (histamine) and negative (saline) controls. What we found was that the reaction, as noted by wheal size, seemed to be significantly blunted following the 11 weeks of supplementation of omega-3 fatty acids, vitamins and trace minerals together with high-quality forage and no grains or concentrates. Some reactions were upwards of over 50 percent smaller than they were when the horses were not supplemented.” The study was then repeated with a pure cold-pressed flax oil infused with vitamin E being added to supplementation. Together these also showed promise in supporting the allergic response.
“Most of my patients are already on a Platinum wellness formula,” says Dr. Gill-Favier of her approach. “If they have seasonal allergies, then I put them on the Platinum Skin & Allergy. I warn my clients that it may take a few weeks to turn their horses around, but it seems to help maintain healthy normal skin."
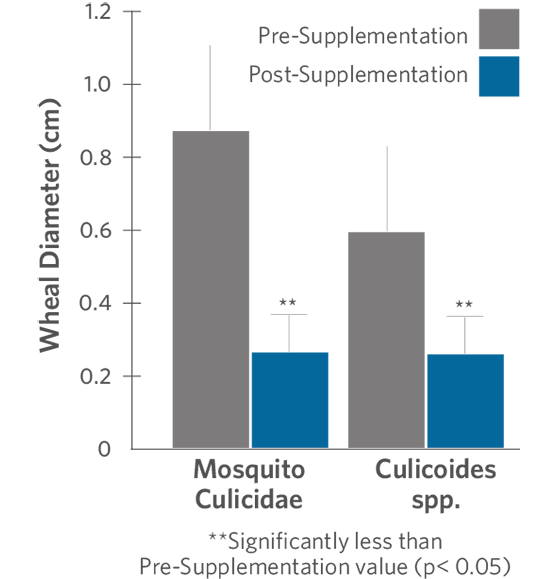
Figure 1. Allergic Response to Mosquito Culicidae and Culicoides spp. Antigens Before and After 11 Weeks Supplementation with Omega-3 Fatty Acids, Vitamins and Trace Minerals
Allergic skin reactions were studied in horses receiving supplementation of omega-3 fatty acids, vitamins and trace minerals. All reactions were signifcantly reduced after 11 weeks of supplementation. For example, the size of wheals that developed in response to injection of a Mixed Grasses antigen was decreased by more than 50 percent in horses ingesting the supplement, when compared to values before supplementation. Furthermore, the mean reaction to the MiteLepidoglyphus Destructor antigen was nearly 40 percent smaller when measured 4-hours after the injection. Similar results were noted in response to the Mosquito Culicidae and Culicoides spp. antigens (Figure 1; 4-hr measurement only).
When ‘Natural’ May Be Better
Targeted nutrition can be significantly effective in supporting a normal allergic response because of its impact on managing oxidative stress and helping to maintain an optimal equine immune system. These nutrients are potent and well-researched tools for veterinarians and horse owners to turn to for long-term results in horses with seasonal allergies. “For me, I would rather take a nutritional approach,” says Dr. Gill-Favier. “I don’t want to have horses on (dexamethasone) all the time; I think it’s dangerous, and especially so with a lot of these horses that are borderline metabolic.” Nutrients can be used as an adjunct to clinical therapies for sustained results, helping a horse’s body to cope without the side-effects often seen with prolonged pharmaceutical intervention. “I think for the long-term you’re actually fixing a problem rather than putting a bandaid on it,” explains Dr. Gill-Favier. “If I can get the job done in a more functional way, and actually solve the problem, then we’re miles ahead. I don’t want to just see the same allergy issues over and over again with pharmaceuticals, but clients also have to understand that it takes time to repair the immune system. It’s not going to turn around overnight.” It’s an approach that Dr. Thaler uses in his patients as well, “I try to get away as much as possible from medication by using management of the situation and also nutrition. Most horses can get there pretty well that way.”
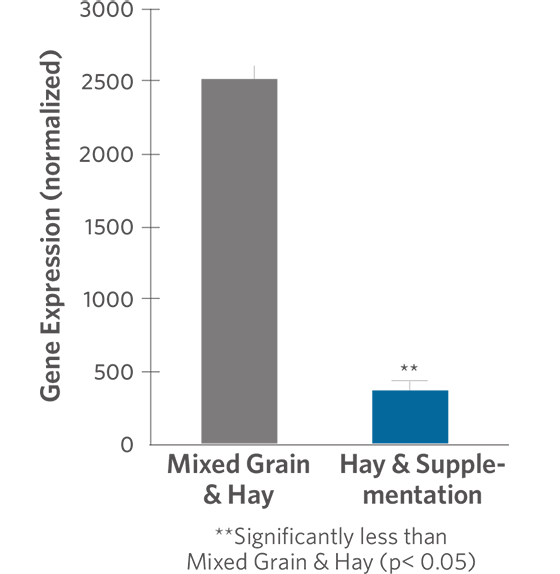
Researchers at the University of California at Davis compared expression of cytokine genes in horses that had been consuming a diet of hay and grain to expression of the same genes in horses fed hay and supplemented with omega-3 fatty acids, vitamins and trace minerals for 6 weeks. Expression of genes for TNF-α and IL-6 were lower by 69 percent and 85 percent, respectively, in the supplemented horses when compared with the non-supplemented horses (Figures 2 and 3). In an observational study conducted by the same research group, horses fed the hay and supplement diet had lower expression of IFN-γ and TNF-α genes than horses eating other feeds (data not shown).
Figure 2. TNF-alpha Gene Expression in Horses Consuming a Hay and Supplemented Diet vs. Horses Consuming Mixed Grain and Hay Diet
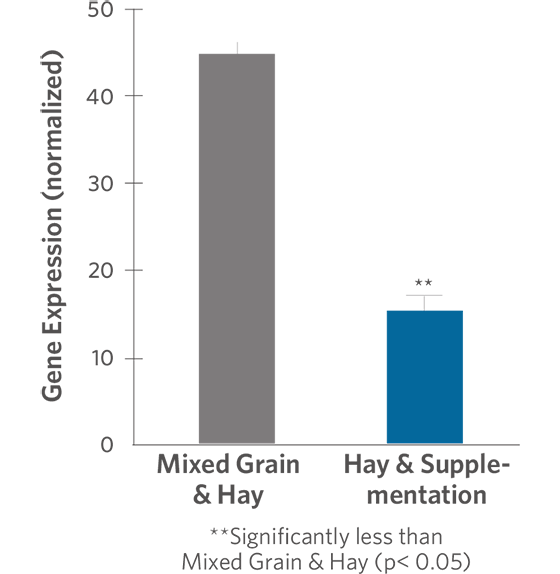
Figure 3. IL-6 Gene Expression in Horses Consuming a Hay and Supplemented Diet vs. Horses Consuming Mixed Grain and Hay Diet
Supporting A Healthy Horse
Aside from their approach to treating equine allergies, these veterinarians share a common commitment to support a horse's total body health. With the use of environmental intervention and nutrition, a large majority of seasonal allergy issues can be avoided before they ever have the opportunity to become clinical. “There’s no one thing,” says Dr. Gill-Favier. “You have to manage the environment, nutrition and take a total holistic approach.” From keeping dust under control to managing insect activity and choosing a high-quality diet together with the right supplements, small steps can lead to significant results. “I remind my clients how much it costs to have me come out to treat their horse for hives compared to how much it costs to practice proactive care and use the Platinum formulas I recommend,” says Dr. Gill-Favier. “That puts things in perspective. I’m trying to help my clients create a program where we have good nutrition, exercise and training programs designed to help support horses for a healthier life.”
The Future
“With additional research into understanding the complex immune mechanisms associated with allergic responses in horses, it will be possible to gain a better understanding of how to manage the clinical manifestations of allergies,” says Meri Stratton-Phelps, DVM, MPVM, DACVIM, (LAIM), DACVN, Veterinary Clinical Nutritionist with Platinum Performance, Inc. “The effect of the gastrointestinal microbiome on the health of the immune system and an improved understanding about the barrier function of equine skin as it relates to atopic dermatitis are important areas of research in the future.” The gut microbiome to which Dr. Stratton-Phelps is referring is seen by many in both veterinary and human medicine to be the so-called ‘next frontier.’ With far-reaching influence on numerous systems in the body, the gut microbiome is thought to affect immune function, metabolic health, allergic response and even play a role in predetermining a human or horse’s propensity for disease. “The gastrointestinal tract is a major component of our immune system with gut microbes playing an instrumental role in immune function and hypersensitivity reactions,” agrees Dr. Hembrooke. “If there is an overabundance of bad microbes, then there could be damage to the intestinal lining and unwanted compounds could enter the systemic circulation. The imbalance could likely lead to an overreaction of the immune system in the way of allergic response. In mouse models, the resident gut microflora and skin barrier status (guided, in part, by the skin microbial balance) influence risk and rates of atopic dermatitis, food allergies, and asthma. Diet-induced changes in other animals have shown alterations of the gut microbiome such that there is an increase in short-chain fatty acid-producing bacteria. This modification is associated with a reduction in asthma incidence via upregulation of Tregs (T cells that down-regulate other immune cells). These diet-induced immune-modulating effects are even transferable to the offspring who show greater resistance to allergies later in life. Furthermore, there is a suggested ‘gut-lung axis’ that is connected via the systemic immune system, which explains how something located in the gastrointestinal tract could affect a distant organ like the lung.”
While it may sound futuristic, research into the advanced impact of the gut microbiome is happening now. Though in its infancy, researchers and practitioners have high hopes for major breakthroughs that will lead to improved treatments and the ability for more proactive care. “We also focus on supporting a normal gut microbiome,” says Dr. Gill-Favier of her practice. “We’re finding out — even stronger in human medicine than in veterinary — that there’s a suspected correlation between allergies, the immune system, auto-immune disease and the gut. It’s a huge deal.” One way to potentially influence the health of the gut microbiome is with the use of probiotics. “Probiotics are known for their ability to establish a healthy gut microbial population that is best suited to maintaining appropriate immune responses,” says Dr. Hembrooke. “Research in humans indicates that probiotics can improve lung function among people with allergic asthma. Population-wide studies suggest probiotics can confer preventive benefits against bronchial asthma and other allergy-associated concerns, while research in other animals also indicates oral probiotics may either prevent or help to treat both skin and respiratory allergic reactions.”
While other aspects of veterinary medicine may be more clearly defined and their treatments more black and white, equine allergies are a gray area that take trial and error combined with tried and true strategies for the most positive outcomes. Much is happening and great hope is on the horizon for significant breakthroughs that could further improve the health, longevity and performance capacity for horses afflicted with skin and respiratory allergies. “In our horses where this is chronic and progressive, if we can decrease their progression, then they can stay where they are longer, and if we can moderate them, then they can have a longer and better quality of life,” says Dr. Swiderski.
Ultimately, it comes down to a greater focus on prevention and a treatment plan with long-term and sustained results as the end goal. Dr. Gill-Favier reminds herself often of why she chooses the approach she does. “The body — whether that’s a human or a horse — has a tremendous capacity to heal if we give it the right tools and get out of the way.”

PHOTO BY ELIZABETH HAY PHOTOGRAPHY
For questions or more information, please email clients@platinumperformance.com or call a Platinum Advisor at (800) 553-2400
For Supportive Literature:
- Fadok, Valerie A. Update on Equine Allergies. Vet Clin Equine 29 (2013) 541-550.
- Jensen-Jarolim et al. Outstanding animal studies in allergy II. From atopic barrier and microbiome to allergen-specific immunotherapy. Curr Opin Allergy Clin Immunol 17 (2017) 180-187

by Jessie Bengoa,
Platinum Performance®

